FINAL PRACTICAL SHORT CASE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
07-06-2022
Hall ticket no. 1701006048
CHIEF COMPLAINTS:
80 years old male , agriculture labourer by occupation came to OPD with the chief complaints of
•FEVER - since 7 days
•Decreased urine output associated with burning micturition since 6 days.
History of presenting illness
Patient is apparently asymptomatic 7 days back, Then he developed fever which is insidious in onset, intermittent with no diurnal variations which relieved on taking medication.
✓ Associated with chills, rigors and generalised body pains.
✓ Associated with an episode of vomiting 2 days back.conent of vomitus is food, which is non bilious, not foul smelling.
✓ No History of cough, cold, shortness of breathe, night sweats.
✓There is burning micturition which is experienced at the start of the urinary flow and relieved after the urination and decreased urine output since 2 days which is not associated with any hematuria.
Past history
He is known case of HYPERTENSION since 24years. Not a known case of diabetes, tuberculosis,asthma and epilepsy.
PAST Surgical history
He underwent a nephrectomy surgery 24yrs ago donated to his brother.
Personal history
Appetite - normal
Diet- mixed
Sleep - adequate
Bowel - constipation is present
Bladder - oliguria since 6 days, associated with burning micturition.
Allergies- none
Addiction- 3 beedi/ day from 27yrs of age
Alcohol- occasionally
Stopped both alcohol and smoking after the nephrectomy surgery.
General examination
Patient is conscious, coherent, co operative and well oriented to time, place, and person moderately build and nourished.
Thereis pallor and pedal edema , but no icterus , cyanosis,clubbing, lymphadenopathy.
Vitals: Febrile 99.2F
BP- 150/90 mmHg ( on medication)
Respiratory rate- 18 cpm
Pulse rate - 76 bpm
Systemic examination:
Abdomen examination:
Inspection:
Umbilicus inverted , No abdominal distention,no visible pulsations,scars and swelling.
PALPATION:
Soft, non tender, no organo megaly.
AUSCULTATION:
BOWEL SOUNDS HEARD
Cardio vascular examination:
No visible pulsations, scars, engorged veins. No rise in jvp
Apex beat is felt at 5 Intercoastal space medial to mid clavicular line.
S1 S2 heard . No murmurs.
- Respiratory system
Shape of chest is elliptical, b/l symmetrical.
Trachea is central. Expansion of chest is symmetrical
Bilateral Airway Entry - positive
Normal vesicular breath sounds
CNS EXAMINATION:
No signs of meningeal signs
Cranial nerves: normal
Sensory system: normal
Motor system: normal
Reflexes: Right. Left.
Biceps. ++. ++
Triceps. ++. ++
Supinator ++. ++
Knee. ++. ++
Ankle ++. ++
Gait: normal.
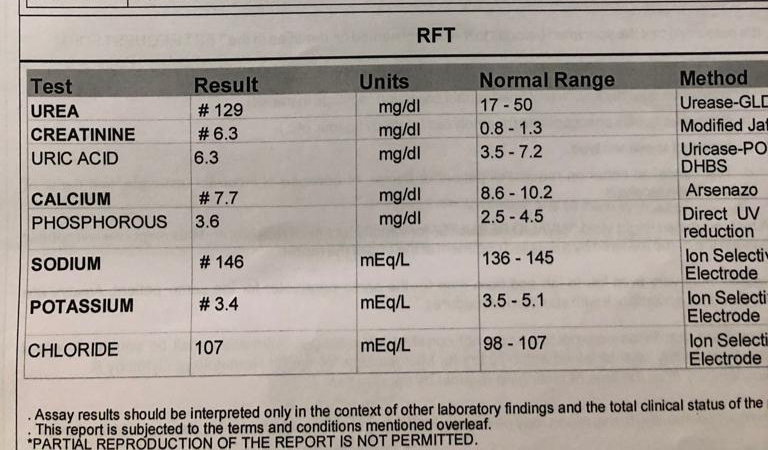
INVESTIGATIONS:
Treatment:
Inj. Piptaz -2.25gm/tid
Tab. Lasix -40ug/po/ bd
Tab. Zofer -4mg/po/ sos
Tab. Dolo -650/ po/ sos
Tab. Pan 40mg /po/ od
Nebi. Duolin and Budecort 6hrly
Syr. Mucaine gel 15ml/po/ bd before meal 15min
Syrup. Cremaffin 15ml/po/ sos.